Why HCPs Prefer Brands with an Automated Buy and Bill Copay Program
Healthcare providers (HCPs) face challenges managing buy and bill programs, from manual copay processes that hinder workflows to reimbursement delays that impact revenue. That is why many practices are increasingly turning to brands with automated buy and bill programs. In this blog, backed by ConnectiveRx's survey data, we'll explore the specific pain points prescribers face with buy and bill and how automation solves them, improving experiences for providers, patients, and drug brands by making the process more efficient and accurate.
Who Are the Key Stakeholders with a Buy and Bill Program?
To start at the beginning, accessing, administering, and paying for specialty drugs presents challenges that often extend far beyond those associated with small-molecule medicines. As a result, manufacturers have deployed an array of support systems to assist key stakeholders. Most of these systems are aimed directly at patients, and rightly so—patients are the ultimate consumers and should be the primary beneficiaries.
But patients aren’t the only stakeholders that face serious obstacles as they attempt to navigate the specialty drug marketplace. Prescribers have their own set of hurdles to jump, especially when working with buy and bill medications. For marketers of brands in the buy and bill space, proper support of prescribers begins with a solid understanding of the unique challenges faced by prescribers in the specialty-drug arena.
4 Pain Points Prescribers Face in Buy and Bill Copay Programs
HCPs face at least four distinct pain points as they manage buy and bill brands:
- Staff must help patients navigate support systems that are not patient friendly: Patient support systems, while deployed with the best of intentions, are often complex and confusing to patients. Further, few brands provide a “one-stop shop” for all of their patient support programs.
- Office support is disjointed: Commonly, a brand’s various physician-facing support programs (e.g., benefits verification, benefits investigation, patient assistance programs, and copay support) are provided by different vendors, leaving office staff with the task of learning and managing systems from multiple sources.
- Gaining patient access to medications is often painfully slow: In many cases, the delay in processing benefits verification, benefits investigation, and prior authorization assistance is so great that treatment selection is impacted.
- The provider is at financial risk for the cost of the products: Buy and bill medications are expensive products that must be on hand when needed. This puts the practice in the position of being a warehouse and distribution center responsible for product ordering, inventory management, billing, and reconciliation. If not managed flawlessly, or if usage falters or shifts to alternative agents, the costs can be profound.
These challenges underscore the immense burden placed on providers, who must balance financial risk with the operational complexities of managing high-cost medications. Without streamlined processes and support systems in place, these pain points can significantly hinder both practice efficiency and patient care.
What Should Brand Managers do to Help Protect Buy and Bill Prescribers?
To help combat these hurdles, brand teams can take several steps to alleviate the four pain points.
- Consolidate support services to reduce complexity. Rather than providing a disjointed set of support services that confuses patients and practices alike, bring these disparate programs together under a single integrated provider.
- Go digital to streamline access. Provide a prescriber-facing hub portal interface from which a prescriber staff member can manage all your brand’s support programs.
- Provide complete office-staff training. Deploy personnel—either on-site or remote—to properly train key prescriber team members on all the facets of the elegant support system you’ve deployed.
ConnectiveRx Buy and Bill Survey Data Results
The strategies laid out above were sourced from two highly credible resources—ConnectiveRx's vast experience in the buy and bill industry and from our recent survey-based research on the role of automation in buy-and-bill programs.
This research focused on the needs of two distinct audiences—prescribers and their staff and pharmaceutical manufacturer brand stakeholders. Below, we report on four of the top-line results of the survey, which uncovers the aspects of copay programs that may create favor of one brand over another. This data was also featured in a guest post on the Drug Channels Institute.
Sneak Peek: Automated processes for buy and bill copay programs drive better HCP, office staff, and patient experiences. As a result, they create a differentiated benefit to brands that deploy them. By automating the copay assistance process for buy-and-bill brands, marketers can promote faster turnaround times, rapid payments, and greater efficiency for the billing process.
Finding #1: In-Workflow Processes Are Paramount
We asked respondents to “select the top three attributes you consider the most important in a copay assistance program for a buy-and-bill product.” The leading responses:
- Process fits in-workflow for my practice
- Rapid turnaround on claims processing and payments
- Username/password-protected provider portal for enrollment, claim submission, tracking, and reports
Clearly, medical practices are over faxing and snail mail. They prefer to manage buy-and-bill copay programs through digital processes that fit in-workflow or can be easily managed through a provider portal. Further, they want fast turnaround on claims submission and payments, which can only be accomplished through technology. In addition to the benefits for practices and patients, automated processes deliver benefits for brands, including automatic data capture, more complete reporting, and better insight into patient adherence.
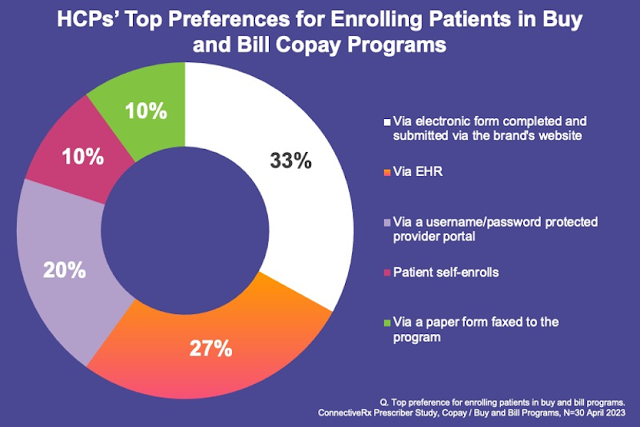
Finding #2: Enrollment Via Website, EHR, Or Portal Is Preferred
Delving into the specific tasks that must be navigated, we asked respondents to “select your/your practice’s top preference for enrolling patients in a buy-and-bill copay program.” The top three responses were all technology-based:
- Via electronic form completed and submitted via the brand’s website
- Via EHR
- Via a username/password-protected provider portal
Physicians and their team members generally want to take responsibility for enrolling patients in buy-and-bill programs, but they have largely moved beyond faxed paper forms. Instead, they want to enroll patients quickly and efficiently through technological means. While the brand’s website is still the top-rated enrollment channel, EHR is growing in popularity and may soon become the most preferred channel because it is in the practice workflow.
Finding #3: Claim Submission Via EHR Or Portal Is Favored Over Fax
Focusing on the claim submission process, we asked survey participants to “select your/your practice’s top preference for submitting claims to buy-and-bill copay programs.” And the bad news for fax and snail mail continues. The leading answers:
- Electronic transmission as a secondary claim via practice EHR billing system
- Upload claim and documentation through a portal that requires username and password
As shown in these responses, the vast majority of prescribers and their teams are looking to streamline claim submission through the use of either their EHR or a brand portal.
Finding #4: Top Payment Preference Is Direct Deposit To The Practice’s Bank Account
Finally, we asked respondents to “select your/your practice’s one preferred method for receiving payment for buy-and-bill copay program claims.” The number one answer, with 50% of responses, was “direct deposit of the payment to the practice’s bank account.” Unsurprisingly, the most technologically advanced and fastest payment method wins the day.
Interestingly, the #2 answer was “patient pays up front and seeks reimbursement from the copay program.” This is an intriguing response, since it suggests that as many as 25% of provider offices may be willing to let patients manage the financial exposure inherent in buy and bill programs.
As shown in the responses to these survey questions, medical practices are eager to adopt automated processes across multiple aspects of copay programs, including enrollment, claim submission, and payment processing. Speed of reimbursement is mission critical and is the most important driver of automation. Providing the path of least resistance and fitting in the office workflow can ultimately drive usage of a brand. Digital processes do more than just benefit provider offices. They can help patients get on and stay on crucial specialty medications.
Automation is the Future of Buy & Bill Copay Programming
In a recent ConnectiveRx webinar, 3 buy and bill experts, including our very own Ticia Cawley, VP of Client Solutions, shared their experiences and opinions on the future of automation in buy and bill copay programming. This was a fast-moving, real-world observation on how automation is (and should be) finding its place in buy & bill programming.
Ticia launched the conversation by reminding the audience that buy and bill copay has moved far beyond the days of 100% manual processes. In fact, today’s buy and bill copay programs can function in a 100% electronic process: paperless from end to end. While it may not be as standardized as the NCPDP pharmacy system, automation is available in buy and bill copay programs.
But, notwithstanding the progress made to date, physicians and staff members are looking for more. Citing our recent survey, as referenced above, Ticia noted that it is “clear that digital solutions and automation are definitely preferred by the prescribers and the prescriber office staff.”
During the one-hour webinar, panelists tackled a series of key questions:
- What should brands be doing to add automation in Buy & Bill program design?
- Should we be prioritizing portals in our push toward automation?
- What are the most effective payment vehicles? Which do you prefer?
- How do we go from a ‘good’ model to a ‘great’ model?
- What are some additional access challenges you face?
- What do you see as the future of Buy & Bill copay?
Interested in the answers to these questions? Tune in to the entire webinar, "Automation and Ease: The Future of Buy and Bill," now!
Frequently Asked Questions about Buy and Bill Copay Program
What is a buy and bill copay program?
A buy and bill copay program is a process where the healthcare provider purchases specialty medications directly from the manufacturer or distributor. The medication is then stored at the practice until it is administered to the patient during their visit. After administration, the provider bills the patient’s insurance for the medication . The copay program helps reduce the out-of-pocket costs for patients, making treatments more affordable and accessible while simplifying the process for both patients and providers.
What are the most common threats to a buy and bill program?
For doctors and office staff, the main threats include reimbursement delays, payer restrictions that create administrative hurdles, and the financial burden of managing expensive inventory. These challenges can increase workload, lead to billing errors, and strain resources.
What are the benefits for a pharma brand to work with buy and bill prescribers?
Working with buy and bill prescribers improves product adoption by ensuring simpler access for patients. It also strengthens provider relationships, increases treatment retention, and generates valuable real-world insights into product usage.
What role does a buy-and-bill copay program play in enhancing patient access?
A buy-and-bill copay program reduces financial barriers for patients by covering part or all of their out-of-pocket costs. This ensures that prescribed therapies remain affordable, particularly for those facing high deductibles or copayments. By easing the financial burden, these programs can improve adherence to treatment plans, ultimately leading to better health outcomes and stronger brand loyalty.
Streamlining Buy and Bill Programs with ConnectiveRx
As the pharma industry increasingly adopts digital processes, it’s essential for copay assistance programs, like buy and bill, to evolve with these changes. Patients and providers need proper support from drug brands to navigate these programs effectively, which can be achieved through education, training, and outreach. At the same time, the shift toward digital and automated solutions, such as electronic benefits verification (eBV), electronic prior authorization (ePA), and electronic copay claim submissions, helps streamline the process. By reducing these burdens, drug brands can enhance satisfaction among prescribers, office staff, and patients while ensuring better adherence to specialty medications. Connect with our buy and bill experts today to learn more.
Automation and Ease: The Future of Buy and Bill
Tune in to our webinar on-demand and join the experts to learn more about the ways in which your brand can support a more streamlined buy and bill program, as reported on by the HCPs and their staff.